Toxic Drugs Are Circulating
In 2016, the Province of British Columbia declared a public health emergency in response to a significant increase in drug-related overdoses and deaths. This toxic drug crisis, primarily driven by a highly potent and unregulated supply of illicit drugs, remains a complex and evolving issue.
Over the past eight years, more than 15,000 lives have been lost in B.C. due to toxic drugs. BC Coroners Service data indicates that First Nations people died of drug poisonings at 6.1 times the rate of other B.C. residents in 2023.
Substances, or drugs, can be defined as something that alters your mental, emotional or physical state. Legal substances, such as alcohol, cannabis, caffeine, prescriptions & nicotine are commonly used. Illegal substances are not regulated and carry higher risks as you may not know the exact contents.
It is important to think about the impacts that substance use can have on your health and wellbeing. There are increased risks associated with using substances. Please consider ways to stay safer if you or someone you know uses drugs or is considering trying drugs for the first time.

Alcohol
What is alcohol?
Alcohol is a depressive substance that can alter your mental, physical and emotional health. Alcohol is a legal substance in Canada and can be purchased in British Columbia by an adult over the age of 19.
Canada's Guidance on Alcohol and Health, defines a standard drink as:
- 1 beer, cooler, cider or premixed cocktail (341mL or 12oz, 5% alcohol); or
- 1 glass of wine (142ml or 5oz, 12% alcohol); or
- 1 drink of distilled alcohol (43ml or 1.5oz, 40% alcohol)

Learn More
How alcohol can impact you
All alcohol has the same effect on the body, and no amount of alcohol is good for your health. The more you drink, the more consequences you could face.
Consuming four or more standard drinks in one setting as a woman, or five or more standard drinks as a man, is considered binge drinking. A high proportion of alcohol consumed by university students is binge drinking, often while celebrating or socializing with friends.
There are significant risks associated with long-term, excessive binge drinking, including developing different types of cancer and an increased risk of heart disease and stroke.
Short-term alcohol use can:
- Impact your judgement, reflexes, and behaviour
- Increase your risk of anxiety, depression, suicide, and other mental health concerns
- Decrease your academic performance
- Increase your risk of injury from violence, accidents, or risky behaviours
- Increase your risk of developing health issues such as cancer and heart disease
Visit the Canadian Centre for Addiction & Mental Health for more information about alcohol’s effects.
Signs of alcohol intoxication and poisoning
If someone consumes an excessive amount of alcohol, they can experience alcohol poisoning. This can lead to irreversible brain damage or death if not treated immediately.
Alcohol Intoxication
- Flushed skin
- Slurred speech
- Staggering gait
- Impaired judgment
- Inability to focus or pay attention
- Reduced inhibition and muscle control
Alcohol Poisoning
- Inability to stand
- Vomiting
- Incontinence
- Clammy skin
- Low body temperature
- Slow or labored breathing
- Passing out or inability to wake
- Seizures
Ways to stay safe and reduce harms while drinking
If you choose to drink alcohol, here are some ways to stay safe:
- Eat food and drink water before and while consuming alcohol
- Choose beverages with lower alcohol content and alternate drinks with water or soda
- Stop drinking before you feel intoxicated
- Drink slowly and avoid drinking games
- Do not mix alcohol with other substances
- Arrange safe transportation home or a safe place to stay overnight
- Do not drink and drive
Additional resources and supports
- Alcohol and Drug Information & Referral Service — 1-800-663-1441
- Government of BC – Help Starts Here
- BC Mental Health & Substance Use Services
- Canada’s Guidance on Alcohol and Health
- Saying When App
Support groups
Vaping and E-cigarettes
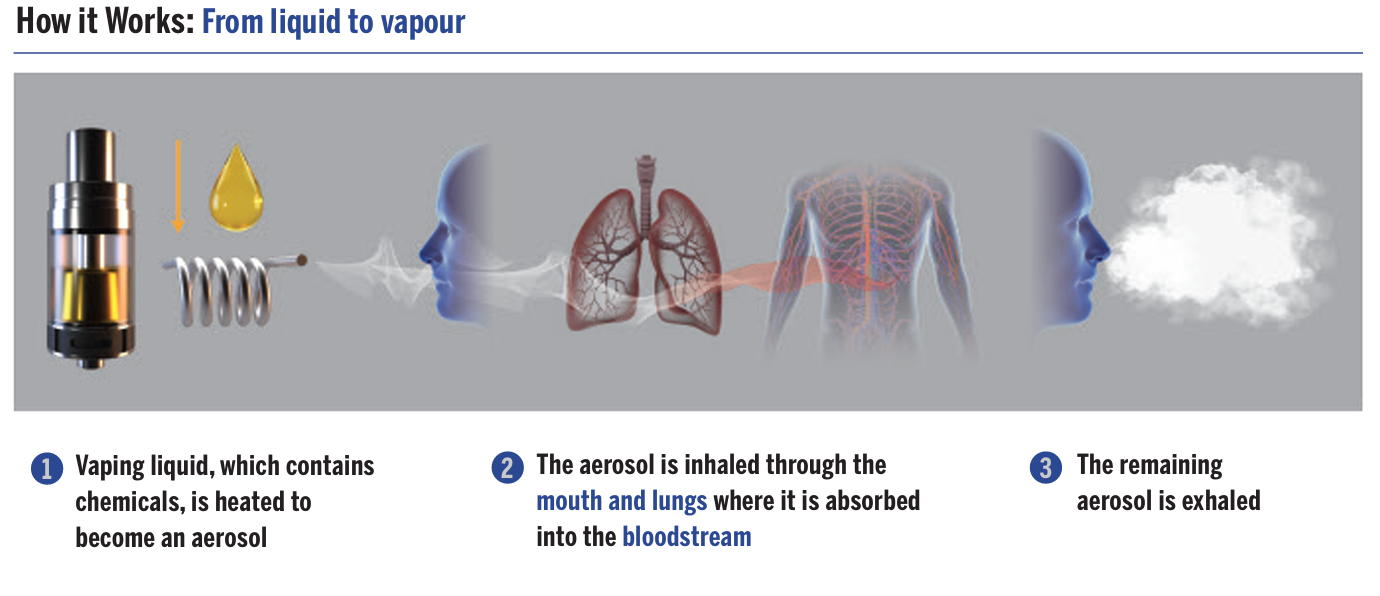
Electronic cigarettes, or vapes, are small, handheld battery-powered devices used to inhale an aerosol. It’s similar to smoking a cigarette, but vaping heats liquid rather than burning tobacco. The term “vaping” can also refer to the inhalation of cannabis. For more information on cannabis, visit Cannabis on Campus.
Vaping devices come in all shapes and sizes.
Types of vaping devices
- Open systems: The vape is filled manually by adding vaping liquid into a tank or pod.
- Closed systems: The device holds a disposable cartridge or pod that is pre-filled with vaping liquid.
Visit Health Canada to learn more about the mechanics of vaping.
Most vaping liquids sold are flavoured and contain nicotine, along with a variety of other chemicals depending on the product. Visit Health Canada for more information about vaping.

Learn More
Nicotine
Nicotine is a highly addictive substance found in tobacco leaves. It releases natural chemicals in your brain that can make you feel more alert, energized or calm. With prolonged use, your body builds a tolerance to some of these effects which can lead to increased use and dependence. Many individuals experience withdrawal symptoms if they go without nicotine for too long. These symptoms go away only after consuming more nicotine or permanently quitting.
Withdrawal symptoms may include:
- Dizziness and shakiness
- Headaches
- Anxiety and irritability
- Nervousness and restlessness
- Difficulty concentrating and sleeping
- Increased appetite
- Slight depression or feeling down
- Cravings for more nicotine
According to Health Canada, most withdrawal symptoms occur during the first week and are usually gone within two to four weeks.
Other health risks
Currently, there is not enough data to know the long-term effects of vaping. However, short term effects include wheezing, shortness of breath and chest pain. Vaping irritates the lungs and airways and can be especially harmful to individuals with underlining health conditions such as asthma. Vaping can also harm the heart by impacting arteries and blood vessels, increase heart rate and blood pressure. Lastly, vaping liquid contains chemicals that are toxic and cancer-causing.
Guidelines and harm reduction
Should you choose to continue vaping despite the risks, these e-cigarette guidelines and recommendations can help you to reduce the risks:
- Do not use unlabelled or old products
- Use your vape device on low heat to reduce inhaling more harmful chemicals
- Be aware of how much nicotine you are consuming to prevent nicotine sickness
- Be careful how you store your vaping device and liquids to prevent nicotine poisoning
- Avoid or limit long term use of vapes
- Maintain your vaping device (clean the vaping tank, change the vape coil regularly, etc.)
- Avoid modifying or reusing disposable vapes
- Store your vape battery carefully to prevent fires or explosions
Smoking cessation
In British Columbia, residents are eligible for a 12-week supply of nicotine replacement therapy (nicotine patches, gum, lozenges) or prescription medication. Nicotine replacement therapy is available at most pharmacies without a prescription. For all prescription medications, please talk to your doctor.
Resources to help you quit smoking or vaping
- HealthLink BC: Quit Smoking
- QuitNow Helpline – a free service with coaches to help you quit and stay smoke-free
- BC Smoking Cessation Program - This program covers the costs of prescription and non-prescription smoking cessation aids for BC residents
- There are two Fraser Health Authority clinics and one Vancouver Coastal Health clinic that provides smoking cessation services to residents in their regions
There are two Fraser Health Authority clinics and one Vancouver Coastal Health clinic that provide smoking cessation services to residents in their regions.
Cannabis
Cannabis, also known as weed, pot, or marijuana, is a plant containing hundreds of chemical substances that affect the brain and body, including THC and CBD. THC is a psychoactive substance found in cannabis. It is responsible for the “high” and intoxicating effects you feel after using cannabis. CBD is another common substance found in cannabis, but it is not psychoactive. CBD is being researched for its possible therapeutic properties. Cannabis can come in many forms, including dried flower/leaves, hash oils, extracts (shatter), edibles, and topical creams. Cannabis products can be smoked, vaped, consumed or applied topically.

Legalization in Canada
On October 17th 2018, the recreational use of cannabis became legal in Canada. One year later, federal cannabis regulations allow the production and sale of edible cannabis products, cannabis extracts and cannabis topicals.
On KPU Campuses
In accordance with KPU’s Smoke Free Campuses and Properties Policy (SR3), smoking and vaping is prohibited on all KPU campuses and properties, including inside private vehicles. This now includes recreational cannabis.
In accordance with KPU’s SR1 Policy, “Students under the influence of alcohol or non-medical drugs must be refused entry to instructional settings if their condition can constitute a hazard to themselves or others”. KPU students are expected to treat recreational cannabis and cannabis products similar to alcohol and other drugs and not come to campus while impaired.
BC Laws

You must be 19 or older to buy, use or grow recreational cannabis.

Recreational cannabis and cannabis products can only be legally purchased at government-run stores, licensed private retailers, or on the online BC store.

Adults can possess 30 grams of dried cannabis, or its equivalent, in public.

Many public spaces in BC do not permit smoking and vaping cannabis, such as parks, bus stops and public buildings.
Opioids
More information coming soon.

If you are looking for treatment for substance use
- If you are looking for treatment for substance use, contact the Opioid Treatment Access Line at 1-833-804-8111. They are open daily, 9 AM to 4 PM, with the last intake at 3:30 PM and voicemail available after hours.
- It is important for you to consider ways to stay safer if you—or someone you know—uses drugs or is considering trying drugs for the first time. No unregulated drug is safe. Prescription medications should also be treated with caution. Visit Help Starts Here for support with reducing or stopping substance use.

Naloxone Kits and Harm Reduction
- If you use or intend to use unregulated drugs, go slowly, pace yourself, and use around other people.
- Sign up for Toxic Drug Alerts in your region by texting the word JOIN to 253787.
- Download the Lifeguard Connect App (Apple App Store or Google Play Store). This app connects you with emergency responders if you or someone you know becomes unresponsive.
- Carry naloxone and sign-up for a free Naloxone training session.
- Consider having your drugs checked.

Naloxone and where you can find it on campus
Naloxone is available at all KPU locations in the event of an emergency:
- KPU Surrey – Maple building & Cedar building
- KPU Langley – East building & West building
- KPU Richmond – First floor Main Building
- KPU Tech – Main Building
- KPU Civic – Level 7 & Level 8
Always call 9-1-1 first in the event of an emergency. Naloxone should be given to an unresponsive person showing signs or symptoms of an overdose. For more information about naloxone, visit KPU First Aid. There are also Emergency Call Buttons across KPU campuses that serve as direct service lines to Security and First Aid.
Drug checking & testing
You can get your drugs tested at supervised consumption sites or overdose prevention sites for free. Visit drugcheckingbc.ca to find access to drug testing and testing strips.
Responding to an accidental opioid poisoning
If you think someone is experiencing an accidental opioid poisoning, call 9-1-1 right away. Stay with that individual until first responders or KPU first aid and security arrive.
Potential signs of an opioid poisoning
- Not moving and can’t be woken up
- Slow breathing or not breathing at all
- Choking, gurgling sounds or even snoring
- Blue lips and nails
- Cold or clammy skin
- Tiny pupils
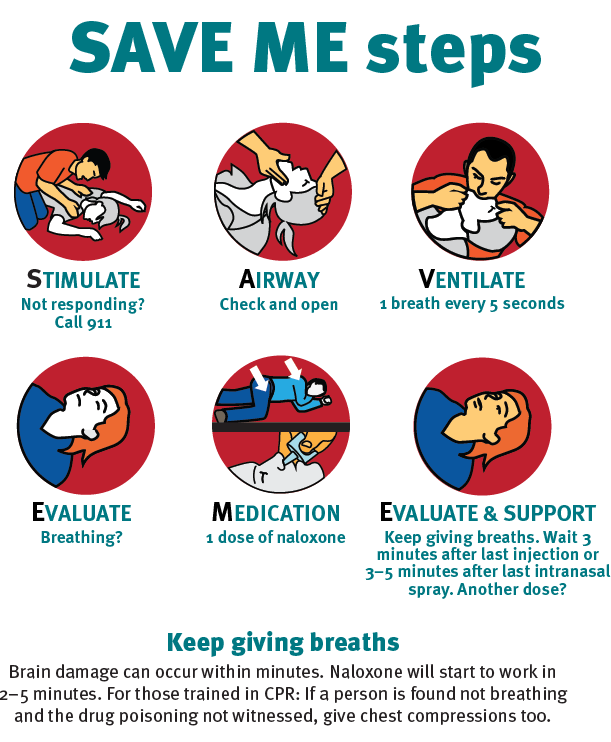
Use the SAVE ME steps to provide aid while you are waiting for help to arrive:
- Stimulate: Not Responding? Call 9-1-1.
- Airway: Check and open.
- Ventilate: One breath every five seconds.
- Evaluate: Breathing?
- Medication: One dose of naloxone.
- Evaluate and support: Keep giving breaths. Wait three minutes after the last injection or three to five minutes after the last intranasal spray. Another dose?
Brain damage can occur within minutes. Naloxone will start to work in two to five minutes. For those train in CPR: if a person is found not breathing and the drug poisoning not witnessed, give chest compressions too.
If you do not know how to administer naloxone or do not have access to it, continue giving breaths until help arrives.
Resources and Workshops
- In an emergency, CALL 9-1-1
- KPU also has Emergency Call Buttons that are a direct link to Security and First Aid across campus.
- Opioid Treatment Access Line: 1-833-804-8111
- BC Alcohol & Drug Information and Referral Service: 1-800-663-1441
- HealthLinkBC or call 8-1-1
- Suicide Crisis Helpline or call 9-8-8
- KUU-US Crisis Line Society or call 1-800-599-8717
- First Nations Health Authority (harm reduction resources)
- Crisis Centre of BC or call 310-6789 (mental health and crisis response)
- TELUS Student Support App (free mental health support for KPU students)
- Here2Talk (free mental health support for BC university students)
- Toward the Heart (information about opioids, naloxone and harm reduction)
- Free Naloxone Training
- Help Starts Here BC (BC health, mental health and wellness services)
- Foundry BC (health and wellness services for young people ages 12-24)
- Respond to Overdose (information on overdose prevention and response)
- Building Better Mental Health and Addiction Care (information and resources on mental health and addictions)

You can learn more about toxic drugs through these Campus Well articles:
Decriminalization
The goal of decriminalizing people who use drugs is to reduce stigma and fear of criminal prosecution that prevents people from reaching out for help, including medical assistance.
Decriminalizing people who use drugs is one of the many actions the government of British Columbia is taking to respond to the toxic drug crisis, so people get the care they need – from prevention and harm reduction to treatment and recovery.
Health Canada granted the province of B.C. a three-year exemption under the Controlled Drugs and Substances Act to decriminalize people who use drugs, which came into effect January 31, 2023.
Under the exemption, possessing small amounts of certain illicit drugs for personal use in specific locations is allowed.
In these locations, adults 18 and older will not be arrested, charged or have drugs seized for possessing small amounts of certain illicit drugs for personal use. Instead, people will be offered health information and referred to treatment and supports if requested.
Learn More
Locations:
- Private residences
- Places unhoused individuals are legally sheltering (indoor and outdoor locations)
- Overdose prevention, drug checking and supervised consumption sites
- Places that provide out-patient addiction services like rapid access addiction clinics
Illicit drugs covered under the exemption (up to 2.5 grams combined):
- Opioids (such as heroin, morphine and fentanyl)
- Crack and powder cocaine
- Methamphetamine (meth)
- MDMA (ecstasy)
What remains illegal
- Adults 18 and older cannot possess:
- More than 2.5 grams combined of the drugs covered under the exemption
- Any amount of other illegal drugs not covered under the exemption
- Any amount of drugs in public places like hospitals, businesses, transit and parks
- Youth under 18 cannot possess any amount of drugs
- Illicit drugs are not legal. They cannot be trafficked or sold in stores
- Drug production, import and export remain illegal, unless authorized under the CDSA
For more information on decriminalization go to: https://www2.gov.bc.ca/gov/content/overdose/decriminalization


The Good Samaritan Act
Saving a life is the number one priority during an opioid poisoning.
The Good Samaritan law protects you from simple drug possession charges and violations of conditions related to parole, probation, conditional sentences or pre-trial release.
This law applies to the person who has overdosed, the person who seeks help and anyone at the scene when help arrives. Visit Health Canada for more information about the Good Samaritan Drug Overdose Act.









